Insoles and the Fight Against Chronic Fatigue Syndrome (CFS)

Chronic Fatigue Syndrome (CFS) is a complex condition characterized by persistent fatigue that does not improve with rest, often accompanied by joint pain, muscle weakness, and overall physical discomfort. While the connection between foot health and CFS may not be immediately apparent, insoles can play a significant role in alleviating some physical stressors associated with the condition. This blog explores how ergonomic insoles enhance posture, balance, and weight distribution, reducing strain on the body and promoting energy conservation.
Understanding Chronic Fatigue Syndrome
Chronic Fatigue Syndrome (CFS), also known as myalgic encephalomyelitis (ME), is a complex and debilitating condition. Characterized by persistent fatigue that does not improve even with rest, it can significantly impact an individual’s quality of life.
Symptoms often extend beyond exhaustion to include joint pain, muscle weakness, and cognitive difficulties. As medical researchers and healthcare providers continue to explore effective treatments, an unexpected yet promising intervention can : the use of foot insoles. By supporting posture and weight distribution on the feet, insoles may offer occasional relief to individuals suffering from this elusive condition.
CFS affects approximately 836,000 to 2.5 million people in the United States alone (Johns Hopkins Medicine, n.d.). Despite its prevalence, diagnosing CFS can be challenging, as there is no single chronic fatigue syndrome test. Instead, healthcare professionals rely on a combination of physical exams and patient-reported symptoms, including unrelenting fatigue lasting more than six months, sleep disturbances, and difficulty concentrating (“Myalgic Encephalomyelitis/Chronic Fatigue Syndrome”, 2023).
What causes chronic fatigue syndrome remains unknown, though various factors like immune system impairments and hormonal imbalances may contribute (Lem, K., Chao, C. Y., & Gabbay, V., 2018). Treatment often involves a combination of lifestyle adjustments and symptom management strategies.
The Link Between Foot Health and CFS
Although foot health may not seem immediately relevant to CFS, it can play a critical role in physical comfort and energy conservation. Many individuals with CFS experience joint pain and musculoskeletal discomfort. When standing or walking places undue stress on the body, it can exacerbate these symptoms, further depleting energy levels (CDCP, 2023).
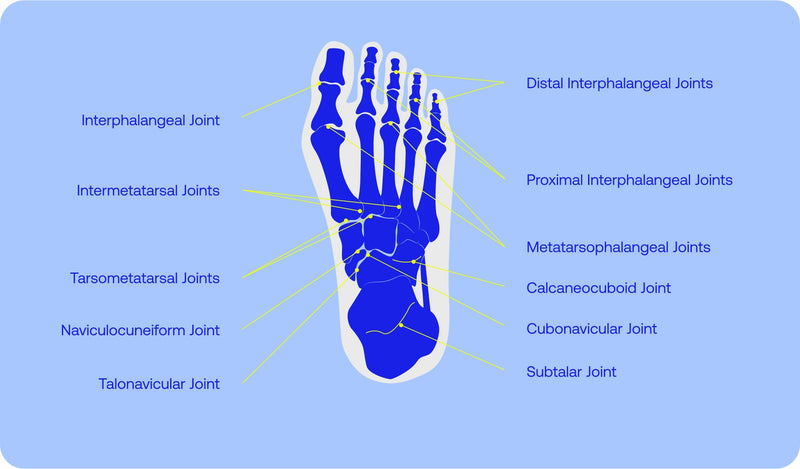
Proper foot alignment facilitated by ergonomic insoles ensures that the body maintains a balanced posture, which can help reduce compensatory movements that often lead to further fatigue. When the feet are correctly supported, the distribution of force during walking or standing becomes more efficient, minimizing unnecessary strain on muscles and joints. This biomechanical advantage not only reduces physical discomfort but also conserves energy—a critical resource for those navigating the daily challenges of CFS.
Ergonomic insoles are designed to enhance posture, balance, and weight distribution. By supporting the natural arches of the feet and cushioning pressure points, insoles can reduce the strain on joints and muscles. This, in turn, can help conserve energy—a crucial consideration for those managing CFS symptoms.
Benefits of Insoles for CFS Management
Incorporating insoles into a holistic chronic fatigue syndrome treatment plan offers several advantages, backed by biomechanical science and practical observations in managing physical stress:
-
Posture Improvement: Maintaining proper posture is critical for overall musculoskeletal health. Poor posture caused by imbalances in the feet places unnecessary strain on the back, hips, and knees, worsening fatigue for individuals with CFS. Insoles help align the body by supporting the natural curvature of the foot, which reduces muscular effort and promotes better spinal alignment.
-
Enhanced Balance: Individuals with CFS frequently report symptoms such as dizziness, vertigo, and instability when standing or walking. This can be attributed to disruptions in proprioception—the body's ability to sense its position in space. Insoles with proper arch support contribute to improved proprioception, enabling better body stability. By reducing compensatory movements, they help individuals feel more secure on their feet and prevent falls or accidents, which can further deplete already limited energy reserves.
-
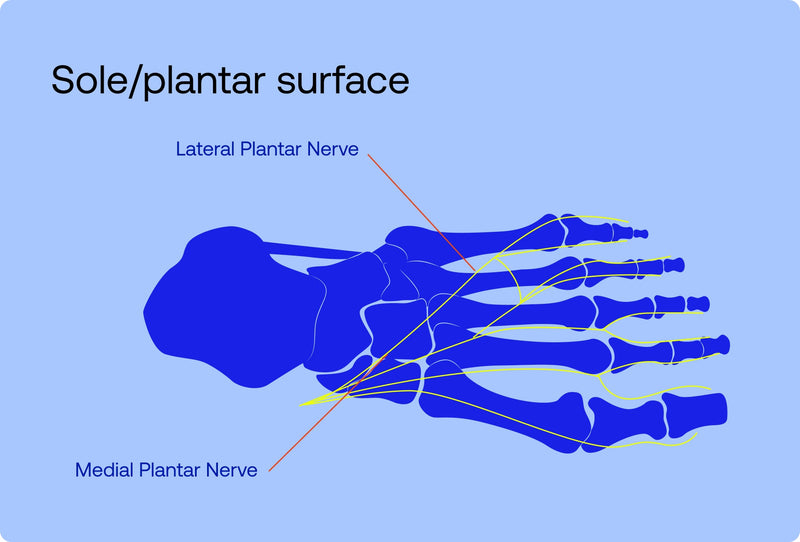
Weight Distribution: Many foot-related problems, including plantar fasciitis and excessive foot fatigue, are linked to uneven weight distribution across the soles of the feet. In people with CFS, uneven pressure points can cause additional discomfort and lead to compensatory movements that exacerbate joint and muscle strain. Insoles promote even weight distribution, which reduces pressure on specific areas of the feet and ensures smoother and more comfortable movement patterns.
-
Posture Improvement: Poor posture increases strain on muscles and joints, leading to unnecessary physical stress. Insoles help align the body, reducing the effort required to maintain proper posture.
Using insoles in general usually requires the following practices to keep up with their overall condition and effectiveness:
1. Gradual Integration: Start by wearing insoles for short periods and gradually increase usage.
2. Footwear Compatibility: Ensure your shoes accommodate the insoles comfortably.
3. Regular Assessment: Periodically evaluate the condition of your insoles to ensure they remain effective.
Holistic Strategies for Beating CFS
Insoles are just one part of the puzzle when it comes to effectively managing symptoms caused by CFS. A well-rounded approach should also include lifestyle adjustments aimed at improving overall well-being and reducing the impact of chronic symptoms.
Nutritional changes, such as adopting an anti-inflammatory diet, can play a role in mitigating fatigue and supporting immune function. Some individuals have explored whether a carnivore diet might help chronic fatigue syndrome by reducing dietary triggers of inflammation, though more research is needed to fully understand its effectiveness.
Additionally, gentle physical activity can be beneficial when carefully managed. Graded Exercise Therapy (GET) may be appropriate for some patients as it involves slowly increasing physical activity levels without triggering symptom flare-ups. However, GET should always be undertaken under medical supervision to avoid exacerbating symptoms. Cognitive Behavioral Therapy (CBT) may also help individuals reframe negative thought patterns and develop coping mechanisms for living with the condition.
Working closely with healthcare professionals who understand what kind of doctor treats chronic fatigue syndrome is essential. A collaborative care team may include primary care physicians, rheumatologists, physical therapists, and nutritionists who work together to provide comprehensive support tailored to each individual's needs.
References
1. Centers for Disease Control and Prevention. (2023). Problems being upright. Retrieved from https://www.cdc.gov/me-cfs/signs-symptoms/index.html#:~:text=Problems%20being%20upright,like%20blurring%20or%20seeing%20spots .
2. Cleveland Clinic. (2023). Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Retrieved from https://my.clevelandclinic.org/health/diseases/17720-myalgic-encephalomyelitis-chronic-fatigue-syndrome-me-cfs
3. Johns Hopkins Medicine. (n.d.). Chronic fatigue syndrome. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-fatigue-syndrome
4. Lem, K., Chao, C. Y., & Gabbay, V. (2018). Chronic fatigue syndrome: Biomechanics and therapeutic interventions. Journal of Medical Rehabilitation, 34(2), 25-32. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5851368/